| Issue |
SICOT-J
Volume 11, 2025
|
|
|---|---|---|
| Article Number | 21 | |
| Number of page(s) | 7 | |
| Section | Knee | |
| DOI | https://doi.org/10.1051/sicotj/2025014 | |
| Published online | 27 March 2025 | |
Original Article
Does the change between the native and the prosthetic posterior tibial slope influence the clinical outcomes after posterior stabilized TKA? A review of 793 knees at a minimum of 5 years follow-up
1
Orthopaedic Surgery and Sports Medicine Department, FIFA Medical Center of Excellence, Croix-Rousse Hospital, Lyon University Hospital, 103 grande rue de la Croix Rousse, 69004 Lyon, France
2
Sydney Orthopaedic Research Institute, University of Notre Dame Australia, Hornsby and Ku-Ring Hospital, Palmerston Rd, Hornsby NSW 2077, Sydney, Australia
3
University of Lyon, Claude Bernard Lyon 1 University, IFSTTAR, LBMC UMR_T9406, 25 Av. François Mitterrand, 69500 Bron, France
4
LIBM – EA 7424, Interuniversity Laboratory of Biology of Mobility, Claude Bernard Lyon 1 University, 4 Rue Raphaël Dubois, 69100 Villeurbanne, France
* Corresponding author: cecile-batailler@hotmail.fr
Received:
23
February
2025
Accepted:
27
February
2025
Introduction: The understanding of the influence of posterior tibial slope (PTS) on knee kinematics has increased. However, the PTS influence on clinical outcomes remains unclear. The study aimed to evaluate whether a significant change between the native and the prosthetic tibial plateau PTS influences functional results and the risk of complications following total knee arthroplasty (TKA). Methods: This was a retrospective, monocentric comparative study. Clinical and radiological data from 793 knees were collected from a prospective surgical database. Inclusion criteria were patients operated with a posterior-stabilized TKA (PS-TKA) for primary tibiofemoral osteoarthritis, with or without associated patellofemoral osteoarthritis, or osteonecrosis of the femoral condyle or tibial plateau, with a minimum follow-up of 5 years. Range of motion and International Knee Society (IKS) score as well as radiological measurements were collected preoperatively and postoperatively at each follow-up visit. Two groups were composed according to the change in PTS between pre- and post-op (Group 1: ≤10°, n = 703; Group 2: >10°, n = 90). Results: The mean follow-up was 75.5 months ± 9.1. The mean change in PTS from preoperative was 4.96° ± 3.24 in group 1 and 12.7° ± 1.87 in group 2. There was no significant difference in the mean IKS Knee subscore (89.5 ± 10.7 and 89.7 ± 10.2, p = 0.89) and mean IKS Function subscore (88.2 ± 15.7 and 86.3 ± 16.6, p = 0.33) in groups 1 and 2, respectively. Postoperative maximum flexion was very satisfactory in both groups with no clinically relevant difference (120.0 ± 11.9 and 123.0 ± 8.3, p = 0.026). The complication rate was 5.0% (n = 40) (5.5% in group 1; 1.1% in group 2; p = 0.07) while the most common complication requiring further procedure was deep infection (n = 9, 1.1%) and the second most common was stiffness (n = 6, 0.8%). Discussion: PTS did not influence postoperative maximum flexion or clinical scores and was not associated with a higher complication rate at a minimum 5-year follow-up after PS-TKA.
Key words: Total knee arthroplasty / Posterior-stabilized / Tibial slope / Knee flexion / Survivorship
© The Authors, published by EDP Sciences, 2025
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Total knee arthroplasty (TKA) is an effective procedure for relieving pain and restoring function in patients with end-stage knee osteoarthritis [1]. While multiple factors contribute to the success of TKA, the role of anatomical variations (coronal, sagittal, and axial alignments) in influencing postoperative outcomes has garnered increasing attention.
The posterior tibial slope (PTS) is the slope of the tibial plateau relative to the longitudinal axis of the tibia and has been implicated in altering knee biomechanics and potentially impacting the functional and clinical results of TKA [2, 3]. It has an indirect role in flexion stability and flexion gap, facilitates femoral rollback and may promote a greater range of motion (ROM). Several biomechanical studies have shown that PTS is positively correlated with the range of flexion [4–6].
The influence of PTS on the ROM or functional outcomes after cruciate-retaining TKA (CR-TKA) [7–9] or posterior-stabilized TKA (PS-TKA) [10–12] has been studied but remains unclear. While some studies propose that modifying tibial slope during TKA can lead to improved kinematics and clinical outcomes [5, 13], others argue that such alterations might introduce an increase in the risk of complications such as implant loosening, instability, and uneven load distribution [7, 10]. Furthermore, follow-up has either been short or limited to small cohorts. There is very limited evidence of the impact of postoperative PTS change on the functional outcome of PS-TKA before 10 years of follow-up.
This study aims to assess the influence of the modification in PTS on clinical outcomes (International Knee Society Score, range of motion, complications, and revisions). We hypothesised that PTS modification of less than 10° would obtain better functional outcomes compared to deviations of than 10°.
Materials and methods
Study design
This retrospective comparative study was conducted at a single institution. Patients who underwent TKA from 1987 to 2016 and received one of two types of PS-TKA implants were identified from a prospective institutional database. A total of 4745 patients were identified, 4116 patients (TORNIER-CORIN©, Montbonnot Saint Martin 38330, France) and 629 patients (AMPLITUDE®, Valence 26000, France).
Patient selection
Inclusion criteria were patients aged over 18 requiring a primary TKA for knee OA or suffering from osteonecrosis of the femoral condyle or tibial plateau. Exclusion criteria were post-traumatic OA, inflammatory arthritis, history of osteotomy, need for tibial tubercle osteotomy (TTO) during the surgery, and patients with a follow-up of less than 5 years. A total of 793 knees were eligible for inclusion (Figure 1). Clinical outcomes were analyzed and divided into two groups according to the modification of PTS (modification by ≤10° in Group 1 and >10° in Group 2). PTS modification was calculated by subtracting the preoperative value from the postoperative value.
 |
Figure 1 Flowchart. |
Seven hundred and ninety-three patients were included in the final analysis. For the analysis, patients were divided into two groups according to the amount of PTS deviation from their native state. In group 1 (≤10°), there were 703 knees; in group 2, there were 90 knees. In the total cohort, the mean age at the index procedure was 69.5 ± 8.46 years and the mean follow-up was 75.5 ± 9.1 months (min = 60; max = 216). Patient demographic information between the two groups is presented in Table 1.
The demographic data between the two groups.
Surgical procedure and rehabilitation
All operations were performed using the same surgical technique, by three experimented surgeons with similar training. All patients received a PS-TKA: Either an Anatomic (AMPLITUDE®, Valence 26000, France) or Kneetec (TORNIER-CORIN©, Montbonnot Saint Martin 38330, France). A trans-quadriceps tendon approach was performed for all patients (medial approach for all varus; lateral approach for all valgus knees as it was described by Verdonk et al. [14] and Gunst et al. [15]). The target postoperative mechanical alignment was neutral with a Hip Knee Ankle (HKA) angle at 180°. It was a measured resection technique with releases, with a goal of symmetric coronal balance. A combination of intramedullary and extramedullary guides was used for the primary tibial cut. An intramedullary guide was used to perform the distal femoral cut with a valgus of 7° in the case of varus deformity and 5° in the case of valgus deformity. In cases of lateral condyle hypoplasia, the femoral component was positioned with 3° of external rotation. Posterior referencing was used to size the femoral component. The tibia was cut with 0° of posterior slope according to the intramedullary guide. Each implant has a built-in posterior slope; 3° in the Anatomic, AMPLITUDE®, and 2.3° in the Kneetec, TORNIER-CORIN© [16, 17]. Patellar resurfacing was performed in 83.3% of cases (661 knees) according to anterior knee pain and patellofemoral osteoarthritis. A standard post-operative physical therapy regimen was initiated following surgery focusing on regaining knee ROM, immediate full weight-bearing and quadriceps strengthening. Manipulation under anaesthesia was performed in patients who failed to progressively regain motion (>90°) with therapy by 8 weeks post-operatively. Arthroscopic arthrolysis was performed in cases of persistent stiffness in flexion, defined by a flexion inferior to 90° after 2 months postoperatively.
Evaluation and outcome variable
Preoperative patient demographics (age, gender, side, height, weight, and body mass index) were collected as well as preoperative and postoperative passive ROM and International Knee Society Score (IKS knee and function) [18]. The patients had a systematic follow-up at 2 months, 1 year, 2 years, 5 years, and every 5 years.
All complications were collected at the last follow-up. A complication was defined as an intercurrent event compromising the functional and vital status and requiring a new consultation or hospitalization.
Radiological measurements were performed preoperatively and postoperatively at each follow-up by a senior surgeon. Digital radiographs were obtained according to the Digital Imaging and Communications in Medicine (DICOM) standards using a calibrated magnification. For each patient, the HKA angle, the femoral and tibial mechanical axis as well and the PTS were measured by an independent orthopaedic surgeon, with an accuracy of 0.1°. On lateral knee radiographs, the longitudinal component of the PTS measurement was determined using a previously described measurement technique that defines the proximal anatomic axis of the tibia on lateral X-ray view [19, 20]. Two lines are drawn: line 1 follows the native lateral tibial plateau (for preoperative measurements) or the prosthetic tibial baseplate (for postoperative measurements); and line 2 connects two points located 5 cm and 15 cm distal to the joint line, midway between the anterior and posterior tibial cortex. The PTS was measured as the angle between line 1 and the perpendicular line to line 2 and subtracted from 90° which gave the value of PTS (Figure 2).
 |
Figure 2 (A) Technique for measuring posterior tibial slope. Two lines are drawn: line 1 follows the native lateral tibial plateau or the prosthetic tibial baseplate; and line 2 connects two points located 5 cm and 15 cm distal to the joint line, midway between the anterior and posterior tibial cortex. The posterior tibial slope was measured as the angle between line 1 and the perpendicular line to line 2. (B) and (C) Case of a change in posterior tibial slope greater than 10°. |
Data analyses
Statistical analysis performed with Medistica©, pvalue.io (graphic user interface to the R statistical analysis software 2019–22). Continuous variables were expressed as their mean and standard deviation. Descriptive data were analyzed using the Student’s t-test for non-categorical variables and the Pearson χ2-test for categorical variables. A p-value of <0.05 was accepted as statistical significance. Survival analysis was performed by the Kaplan-Meier method, with any implant revision as endpoints.
Results
The IKS score rose from 123 ± 27.5 before surgery to 177 ± 22.5 at the last follow-up, with a statistically significant improvement at mid-term follow-up in both groups. The mean PTS changed from 7.4 ± 3.86° to 1.6 ± 1.7° (p < 0.001).
Preoperative and postoperative functional scores and radiological analysis between the two groups are shown in Table 2. The groups were similar for all preoperative characteristics except for the mean PTS (6.6 ± 3.2 vs. 13.6 ± 2.4 in groups 1 and 2 respectively, p < 0.001). There was a statistically significant difference in the mean postoperative PTS (1.6° ± 1.7 vs. 0.9° ± 1.8 in groups 1 and 2 respectively, p < 0.001), but the difference was not clinically relevant.
Preoperative and postoperative clinical and radiological assessment between both groups.
There was no significant difference in mean IKS Knee subscore (89.5 ± 10.7 and 89.7 ± 10.2, p = 0.89) and IKS Function subscore (88.2 ± 15.7 and 86.3 ± 16.6, p = 0.33) in groups 1 and 2 respectively. Postoperative maximum flexion was satisfactory in both groups with no clinically relevant difference (120° ± 11.9° and 123° ± 8.3°, p = 0.026). While there is a statistically significant difference between the two groups, the difference of 3° is not clinically relevant.
The overall complication rate was 5.0% (n = 40) as shown in Table 3 (5.5% in group 1; 1.1% in group 2; p = 0.07). There were 34 patients (4.3%) requiring an additional procedure (group 1: n = 33; group 2, n = 1), and for 16 patients (2.0%) a revision of the femoral and/or tibial component was necessary (all in group 1). The overall survival rate of the total cohort was 95.5% (CI95% 94.0–97.0), and 95.1% (CI95% 93.4–96.8) in group 1 versus 98.9% (CI95% 96.7–100.0) in group 2 (p = 0.12) (Figure 3). The most common cause of reoperation was deep infection (n = 9, 1.1%) followed by stiffness (n = 6, 0.8%) and aseptic loosening (n = 5, 0.6%). There were seven cases of loosening, one for septic reason (femoral component) and six considered as aseptic, including three tibial loosening, and three patellar buttons loosening.
 |
Figure 3 Survival analysis in both groups according to Kaplan Meier, with any implant revision as endpoints. Red curve: the group where PTS change ≤ 10°. Blue curve: the group where PTS change of > 10°. |
Complications in both groups.
Discussion
There is abundant but conflicting literature on the relationship between tibial slope and maximum flexion achieved after PS-TKA. However, to the best of our knowledge, no previous studies have evaluated the clinical consequences of altering the native tibial slope. Contrary to our hypothesis, a change of more than 10° in the native tibial slope with a PS prosthesis did not have a deleterious effect on the medium-term results.
A wide range of native PTS has been reported in patients with knee OA. Hofmann et al. have reported that the normal PTS is 7° [21], between 8°−10° by Laskin and Rieger [22], and 14° by Chiu et al. [23]. Studies have reported differences of up to 5°, and interindividual (medial and lateral posterior tibial slopes) ranges as high as 30° [24]. Despite these observations, the clinical consequences of deviations from the native state following TKA remain unclear.
The correct target for setting the posterior slope in TKAs remains debated. Both the choice of implant design and alignment philosophy affect the PTS slope target. In primary TKA the target PTS varies between 3° and 7° [24]. In PS-TKA, a PTS between 0° and 3° is typically recommended to provide tibial component stability and avoid excessive posterior compressive strains and flexion instability, and these guidelines were followed in our population [25]. With cruciate-retaining implant design, an angle up to 5°–7° can be aimed to achieve adequate ROM, particularly in flexion [26].
The difference between the two groups in postoperative maximum flexion was statistically significant (120.0 ± 11.9 and 123.0 ± 8.3, p = 0.026). However, the difference of 3° is not clinically relevant in this study. Radhamony et al. [27] showed that a change in the PTS does not affect the postoperative ROM in PS-TKR using navigation assists used in their population of 120 knees. They were divided into three groups according to the difference in PTS (Group 1: 0–7.5; Group 2: 7.6–15 and Group 3: 15.1–22.5). The mean difference in the PTS in the three groups was 4.5°, 10.8°, and 18.0°, and there was no statistically significant change in ROM with that of change in PTS. Another prospective randomized controlled study with 31 consecutive patients underwent TKA using a cutting block and intramedullary cutting guide designed to impart a 0-degree posterior tibial slope (group 1) and a 5-degree tibia cutting block was used in 30 subsequent patients (group 2) with a posterior cruciate–sacrificing design. With a minimum 3-month follow-up, they revealed that PTS did not have any effect on post-operative maximal flexion or Hospital for Special Surgery functional score [10]; with a mean postoperative flexion was 123.3° in group 1 (range: 90°–135°) and 119.6° in group 2 (range: 75°–135°). However, they did not exactly analyze the influences of the modification of PTS from the native one, and they focused only on the very short term. Only one retrospective cohort study with long-term (mean follow-up of 9 years) reported the impact of the PTS on postoperative flexion. They evaluated 65 knees who underwent TKA with a PS prosthesis and were divided into the following three groups according to the measured tibial slopes in postoperative: Group 1: ≤4°, Group 2: 4°–7° and Group 3: >7° [12]. They demonstrated a positive significant difference in increasing PTS regarding the maximal flexion in PS-TKA [12]. They found that an increase of 1° of PTS can lead to 1.8° greater flexion.
This study did not show any correlation between PTS change and IKS knee or function scores at the last follow-up. These results are similar to the literature. Kansara and Markel [10] did not find a correlation between PTS change and Hospital for Special Surgery functional score at a minimum of 3 months follow-up in a prospective randomized controlled study. The design of knee prosthesis (PCL-retaining vs. PCL-sacrificing) is an important factor that should be considered in evaluating the relationship between PTS and TKA outcomes. Catani et al. [4] have conducted a biomechanical study showing that PTS is positively correlated with the range of flexion and inhibits excessive tension in the posterior cruciate ligament (PCL) during knee flexion. The fear of excessive PTS is to lead to anterior dislocation of the tibia and biomechanical changes of the knee, compromising the longevity of TKA.
Contrary to our hypothesis, there was no statistically clinically significant difference in comparison between pre- and postoperative modification in ROM, functional score, and any correlation regarding complication among the two groups.
The main limitations of this study include its retrospective design on a large period of inclusion, with a mechanical alignment and measured resection technique. However, this study has the merit of being homogeneous and the largest we are aware of, including a focused analysis of the modification of PTS in PS-TKA at a minimum follow-up of 5 years. One of the limitations of our study is that factors such as the posterior condylar offset were not taken into consideration, which can affect the postoperative ROM. Another limitation is the large difference in sample size between the two groups. Nevertheless, a better understanding of the effect of tibial slope changes in PS-TKA is warranted. Nonetheless, a reduction in PTS may also lead to a decrease in the flexion ROM of the knee [12]. Hence, the degree of reduction in the PTS and its impact on postoperative outcomes deserves further prospective comparative studies with large populations to confirm these results. Then, no power analysis was performed at the beginning of the study.
Conclusion
PTS did not influence postoperative maximum flexion or clinical scores and was not associated with a higher complication rate at a minimum 5-year follow-up after PS-TKA.
Funding
This research did not receive any specific funding.
Conflicts of interest
HA, ED, JS: certified that they have no financial conflict of interest in connection with this article.
CB: Consultant for Groupe Lepine, Stryker, Smith and nephew.
SL: Royalties from Stryker, Consultant for Groupe Lepine and Serf, Advisory board for JBJS Am, European Knee Society, SFHG.
ES: Consultant for Smith and Nephew.
Data availability statement
Data are not available.
Author contribution statement
HA: Conceptualization, Methodology, Data management, Statistics analysis, Literature reviewing, Writing – original draft.
ED: Conceptualization, Methodology, Statistics analysis, Writing – original draft.
JS: Article Editing, Validation.
CB: Methodology, Literature reviewing, Article editing, Validation.
SL: Article editing, Validation.
ES: Conceptualization, Methodology, Article editing, Validation, Supervision.
Ethics approval
All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee, the 1964 Helsinki Declaration and its later amendments, or comparable ethical standards. Data collection and analysis were carried out in accordance with MR004 Reference Methodology from the Commission Nationale de l’Informatique et des Libertés (Ref. 2229975V0) obtained on 6 May 2023. The study was registered and filed on the Health Data Hub website.
Informed consent
Written informed consent was obtained from all patients and/or families.
References
- Wylde V, Dieppe P, Hewlett S, Learmonth ID (2007) Total knee replacement: is it really an effective procedure for all? Knee 14, 417–423. [Google Scholar]
- Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 86, 506–511. [PubMed] [Google Scholar]
- Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76, 745–749. [PubMed] [Google Scholar]
- Catani F, Leardini A, Ensini A, Cucca G, Bragonzoni L, Toksvig-Larsen S, Giannini S (2004) The stability of the cemented tibial component of total knee arthroplasty: posterior cruciate-retaining versus posterior-stabilized design. J Arthroplasty 19, 775–782. [PubMed] [Google Scholar]
- Chambers AW, Wood AR, Kosmopoulos V, Sanchez HB, Wagner RA (2016) Effect of posterior tibial slope on flexion and anterior-posterior tibial translation in posterior cruciate-retaining total knee arthroplasty. J Arthroplasty 31, 103–106. [PubMed] [Google Scholar]
- Wang Y, Yan S, Zeng J, Zhang K (2020) The biomechanical effect of different posterior tibial slopes on the tibiofemoral joint after posterior-stabilized total knee arthroplasty. J Orthop Surg Res 15, 320. [Google Scholar]
- Fujimoto E, Sasashige Y, Masuda Y, Hisatome T, Eguchi A, Masuda T, Sawa M, Nagata Y (2013) Significant effect of the posterior tibial slope and medial/lateral ligament balance on knee flexion in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21, 2704–2712. [Google Scholar]
- Howard JL, Morcos MW, Lanting BA, Somerville LE, McAuley JP (2020) Reproducing the native posterior tibial slope in cruciate-retaining total knee arthroplasty: technique and clinical implications. Orthopedics 43, e21–e26. [Google Scholar]
- Malviya A, Lingard EA, Weir DJ, Deehan DJ (2009) Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope. Knee Surg Sports Traumatol Arthrosc 17, 491–498. [Google Scholar]
- Kansara D, Markel DC (2006) The effect of posterior tibial slope on range of motion after total knee arthroplasty. J Arthroplasty 21, 809–813. [PubMed] [Google Scholar]
- Lee OS, Lee J, Lee MC, Han HS (2023) Effect of posterior tibial slope change on postoperative range of motion and clinical outcomes after posterior cruciate-substituting total knee arthroplasty. J Knee Surg 36, 87–94. [Google Scholar]
- Shi X, Shen B, Kang P, Yang J, Zhou Z, Pei F (2013) The effect of posterior tibial slope on knee flexion in posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21, 2696–2703. [Google Scholar]
- Kang KT, Koh YG, Son J, Kwon OR, Lee JS, Kwon SK (2018) Influence of increased posterior tibial slope in total knee arthroplasty on knee joint biomechanics: a computational simulation study. J Arthroplasty 33, 572–579. [Google Scholar]
- Verdonk PC, Pernin J, Pinaroli A, Ait Si Selmi T, Neyret P (2009) Soft tissue balancing in varus total knee arthroplasty: an algorithmic approach. Knee Surg Sports Traumatol Arthrosc 17, 660–666. [Google Scholar]
- Gunst S, Villa V, Magnussen R, Servien E, Lustig S, Neyret P (2016) Equivalent results of medial and lateral parapatellar approach for total knee arthroplasty in mild valgus deformities. Int Orthop 40, 945–951. [Google Scholar]
- Demey G, Magnussen RA, Lustig S, Servien E, Neyret P (2012) Total knee arthroplasty for advanced osteoarthritis in the anterior cruciate ligament deficient knee. Int Orthop 36, 559–564. [Google Scholar]
- Gaillard R, Lustig S, Peltier A, Villa V, Servien E, Neyret P (2016) Total knee implant posterior stabilised by a third condyle: Design evolution and post-operative complications. Orthop Traumatol Surg Res 102, 1061–1068. [Google Scholar]
- Debette C, Parratte S, Maucort-Boulch D, Blanc G, Pauly V, Lustig S, Servien E, Neyret P, Argenson JN (2014) French adaptation of the new Knee Society Scoring System for total knee arthroplasty. Orthop Traumatol Surg Res 100, 531–534. [CrossRef] [PubMed] [Google Scholar]
- Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK (2008) Anatomical references to assess the posterior tibial slope in total knee arthroplasty: a comparison of 5 anatomical axes. J Arthroplasty 23, 586–592. [PubMed] [Google Scholar]
- Bernhardson AS, DePhillipo NN, Aman ZS, Kennedy MI, Dornan GJ, LaPrade RF (2019) Decreased posterior tibial slope does not affect postoperative posterior knee laxity after double-bundle posterior cruciate ligament reconstruction. Am J Sports Med 47, 318–323. [Google Scholar]
- Hofmann AA, Bachus KN, Wyatt RW (1991) Effect of the tibial cut on subsidence following total knee arthroplasty. Clin Orthop Relat Res 269, 63–69. [Google Scholar]
- Laskin RS, Rieger MA (1989) The surgical technique for performing a total knee replacement arthroplasty. Orthop Clin North Am 20, 31–48. [PubMed] [Google Scholar]
- Chiu KY, Zhang SD, Zhang GH (2000) Posterior slope of tibial plateau in Chinese. J Arthroplasty 15, 224–227. [PubMed] [Google Scholar]
- Calek AK, Hochreiter B, Hess S, Amsler F, Leclerq V, Hirschmann MT, Behrend H (2022) High inter- and intraindividual differences in medial and lateral posterior tibial slope are not reproduced accurately by conventional TKA alignment techniques. Knee Surg Sports Traumatol Arthrosc 30, 882–889. [Google Scholar]
- Bai B, Baez J, Testa N, Kummer FJ (2000) Effect of posterior cut angle on tibial component loading. J Arthroplasty 15, 916–920. [PubMed] [Google Scholar]
- Naendrup JH, Drouven SF, Shaikh HS, Jaecker V, Offerhaus C, Shafizadeh ST, Pfeiffer TR (2020) High variability of tibial slope measurement methods in daily clinical practice: Comparisons between measurements on lateral radiograph, magnetic resonance imaging, and computed tomography. Knee 27, 923–929. [Google Scholar]
- Radhamony NG, Chaugule A, Bhende HS (2022) The relationship between posterior tibial slope and knee range of movements in posterior stabilized total knee replacement: a navigation-assisted analysis of 120 cases. Cureus 14, e29695. [PubMed] [Google Scholar]
Cite this article as: Alhamdi H, Deroche E, Shatrov J, Batailler C, Lustig S & Servien E (2025) Does the change between the native and the prosthetic posterior tibial slope influence the clinical outcomes after posterior stabilized TKA? A review of 793 knees at a minimum of 5 years follow-up. SICOT-J 11, 21. https://doi.org/10.1051/sicotj/2025014.
All Tables
Preoperative and postoperative clinical and radiological assessment between both groups.
All Figures
 |
Figure 1 Flowchart. |
| In the text | |
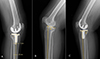 |
Figure 2 (A) Technique for measuring posterior tibial slope. Two lines are drawn: line 1 follows the native lateral tibial plateau or the prosthetic tibial baseplate; and line 2 connects two points located 5 cm and 15 cm distal to the joint line, midway between the anterior and posterior tibial cortex. The posterior tibial slope was measured as the angle between line 1 and the perpendicular line to line 2. (B) and (C) Case of a change in posterior tibial slope greater than 10°. |
| In the text | |
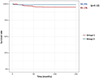 |
Figure 3 Survival analysis in both groups according to Kaplan Meier, with any implant revision as endpoints. Red curve: the group where PTS change ≤ 10°. Blue curve: the group where PTS change of > 10°. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


