| Issue |
SICOT-J
Volume 11, 2025
|
|
|---|---|---|
| Article Number | 33 | |
| Number of page(s) | 6 | |
| Section | Knee | |
| DOI | https://doi.org/10.1051/sicotj/2025018 | |
| Published online | 06 June 2025 | |
Original Article
Rotating-platform deep-dish total knee arthroplasty with restricted kinematic alignment: Five-year clinical and functional outcomes
1
Department of Orthopedic Surgery and Sport Medicine, Croix-Rousse Hospital, FIFA Medical Center of Excellence, 69004 Lyon, France
2
Department of Orthopedic Surgery, Ghent University Hospital, 9000 Ghent, Belgium
3
EA 7424, Interuniversity Laboratory of Human Movement Science, Université Lyon 1, 69003 Lyon, France
4
Université de Lyon, Université Claude Bernard Lyon 1, IFSTTAR, LBMC UMR_T9406, 69622 Lyon, France
* Corresponding author: cecile.batailler@chu-lyon.fr
Received:
4
March
2025
Accepted:
15
March
2025
Introduction: Total knee arthroplasty (TKA) utilizing deep-dish tibial inserts has gained interest due to its high congruency and enhanced stability. However, due to the advent of more personalized alignment philosophies, the combination of a rotating-platform deep-dish TKA design with restricted kinematic alignment (rKA) might improve patient satisfaction. Therefore, this study evaluated the five-year clinical and functional outcomes of rKA with a deep-dish TKA design. Methods: A retrospective analysis was conducted on patients who underwent primary TKA with a rotating-platform deep-dish design and rKA. Of 143 eligible patients, 123 completed five-year follow-up. Clinical and radiographic assessments included the five-year postoperative results: Knee Society Score (KSS), patient satisfaction, range of motion, coronal limb and implant alignment, postoperative complications and implant survivorship. Statistical analyses compared preoperative and postoperative outcomes with paired analyses. Results: Median KSS Knee and Function scores significantly improved from 70 (IQR 5) and 60 (IQR 26) preoperatively to 90 (IQR 20) and 93 (IQR 21) postoperatively (p < 0.001). Postoperative coronal alignment in this study encompassed a hip-knee-ankle angle was 178.1° ± 3.5, a Lateral Distal Femoral Angle of 89.9° ± 2.6, and a Medial Proximal Tibial Angle of 88.6° ± 2.2. At five years, 94% of patients were either satisfied or very satisfied. The revision-free survival rate was 98%. Periprosthetic joint infection and arthrofibrosis were the most common complications (1.6% for both groups separately), followed by aseptic loosening of a cementless femoral component (0.8%) and patellar dislocation (0.8%). Discussion: Rotating-platform deep-dish TKA with restricted kinematic alignment results in excellent functional outcomes, high patient satisfaction, and low complication rates at five-year follow-up. These findings support its viability as a surgical strategy, though long-term studies are warranted to assess implant durability and survivorship beyond 10 years.
Key words: Deep-dish / Rotating platform / TKA / Restricted kinematic alignment
© The Authors, published by EDP Sciences, 2025
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Total knee arthroplasty (TKA) is a widely utilized surgical intervention aimed at alleviating pain and restoring function in patients with advanced knee arthritis. Among various TKA designs, deep-dish tibial inserts, characterized by their high congruency and enhanced anterior-posterior stability, are a viable option [1–3]. These inserts aim to optimize joint stability and improve postoperative outcomes without compromising mobility.
Deep-dish TKA designs have demonstrated equivalent short-term early postoperative functional outcomes when compared to standard posterior-stabilized (PS) or cruciate-retaining (CR) designs [2, 3]. For instance, Shatrov et al. reported no significant difference in clinical outcomes and range of motion (ROM) between patients undergoing condylar-stabilized deep-dish TKA and posterior-stabilized designs at short-term follow-up, emphasizing their utility as a versatile alternative [2]. Similarly, Stadler et al. highlighted the mid-term durability of cementless deep-dish TKA, showing excellent implant survival and negligible aseptic loosening at five years [4].
Similar to the different TKA designs possibilities there are several different strategies to position the femoral and tibial components [5]. Kinematic alignment focuses on restoring pre-arthritic alignment [6]. This method reduces the need for soft tissue releases and aims to preserve normal knee kinematics, which may potentially improve functional outcomes and patient satisfaction. However, there is an ongoing debate about the long-term implications of KA in TKA, particularly with respect to the difficulty restoring the pre-arthritic states and issues regarding patellofemoral tracking with implants designed for mechanical alignment [7–9]. As such, the concept of restricted kinematic alignment (rKA) has been proposed, which involves limiting the alignment within a narrower range of anatomical constraints. The restrictions in rKA could enhance the longevity of the implant and optimize its biomechanical behavior by more closely mimicking the natural joint mechanics [10]. While deep-dish TKA has demonstrated promising early outcomes, little is known about its performance in the context of restricted kinematic alignment over longer follow-up periods. This personalization of implant alignment along with the high congruency provided by the implant might further improve clinical outcomes and patient satisfaction in patients receiving TKA. As such, this study evaluates the five-year clinical and functional outcomes of rotating-platform deep-dish TKA with restricted kinematic alignment.
Materials and methods
This retrospective study was conducted at a single tertiary arthroplasty center, analyzing patients who underwent deep-dish total knee arthroplasty for end-stage osteoarthritis in 2018 and 2019.
Inclusion criteria were: all patients receiving primary TKA for end-stage osteoarthritis, use of a rotating-platform deep-dish TKA design, and minimum postoperative follow-up of five years. Exclusion criteria were: collateral ligamentous insufficiency, severe extra-articular deformities (>10°) requiring corrective osteotomies, post-traumatic arthritis with substantial bone loss, and history of infection, incomplete radiographic and clinical follow-up. Ethics approval was obtained from our institutional ethics committee (ICP-D106.02). Written informed consent was obtained from all patients and/or families. Of the 143 patients eligible to the in- and exclusion criteria, 14 were lost-to follow-up in the hospital prior to completion of the 5-year follow-up. Five patients died during the follow-up period. The demographics of all patients included in the study can be found in Table 1.
Patient demographics.
Surgical technique
All procedures were performed by a fellowship-trained arthroplasty surgeon using a standardized approach, with a rotating-platform deep-dish design (Score 2, Amplitude, and Valence, France). Tourniquet was not used throughout the study. In case of varus osteoarthritis, a subvastus approach was performed, whereas a lateral parapatellar approach was performed in case of valgus osteoarthritis (Hip-Knee-Ankle angle (HKA) > 183°). A restricted kinematic alignment philosophy was used to perform the bony cuts and position the femoral and tibial implants [11]. The tibial and, in case of patellar resurfacing, the patellar components were cemented. The femoral component was either cemented or cementless, based on the bone quality of the patient, as assessed preoperatively on radiographs or intraoperatively. In total 10% of patients received a cementless femoral implant. Local infiltration analgesia with a combination of ropivacaine, epinephrine, and clonidine was administered intraoperatively. Patellar resurfacing was performed selectively, based on intraoperative cartilage quality, Iwano classification grade 2 or higher, and preoperative symptoms.
Postoperative management
All patients underwent the same postoperative rehabilitation protocol. Early mobilization was encouraged, with weight-bearing as tolerated starting on postoperative day one. Physiotherapy included range-of-motion exercises, quadriceps strengthening, and gait training. Patients were discharged when they achieved adequate pain control, independent mobility, and knee flexion of at least 90°.
Outcomes assessed
Patients received routine follow-up at 2 months, 1 year and 5 years. In case of any irregularity or patient concern, earlier follow-up was scheduled. The following variables were collected: Demographic data, including age, sex, body mass index (BMI), Charnley classification, and Devane classification [12, 13]. Clinical and functional assessment was evaluated using the Knee Society Score (KSS), including both the Knee and Function subscales (0: worse, 100: best) [14]. As well, the HKA, Mechanical Medial Proximal Tibial Angle (mMPTA), Mechanical Lateral Distal Femoral Angle (mLDFA), Blackburn-Peel index, patellar tilt and patellar mediolateral position were analyzed on full leg standing radiographs, anteroposterior (AP), lateral and axial knee views. Complications were recorded during follow-up. More specifically, surgical site infection or periprosthetic joint infection (PJI) were diagnosed based on the Musculoskeletal Infection Society criteria [15]. Other complications such as hematoma, aseptic loosening, periprosthetic fracture, arthrofibrosis, instability, and patellar issues were defined based current literature [16, 17]. Survivorship analysis was based on revision TKA for any cause.
Statistical analysis
SPSS (Version 23, IBM, USA) was used for all statistical analyses. Shapiro-Wilk tests were used to verify normality of the data, which was visually verified with boxplots. Continuous variables are presented as means and standard deviations (SD) in the case of parametric data, and median with interquartile range (IQR) in case of non-parametric data. Comparisons between preoperative and postoperative outcomes were analyzed using paired t-tests in case of parametric data, whereas otherwise the non-parametric Wilcoxon test was used. Categorical variables were reported as frequencies and percentages. Kaplan-Meier analysis was used to evaluate implant survivorship. A p-value of <0.05 was considered statistically significant.
An a priori sample size calculation was performed with GPower (Version 3.1, Heinrich Heine University, Düsseldorf, Germany) based on a minimally clinical important difference in KSS Knee score of 6.6 (SD 24.0) with a power of 80% and an alpha level of 0.05 [18]. This analysis determined that 106 subjects were required to achieve sufficient statistical power.
Results
At 5 years of follow-up 94% were either satisfied (49%) or very satisfied (45%) with their postoperative result. Six percent of patients were dissatisfied at 5 years postoperative. The median KSS Knee scores improved from 70 (IQR 5) preoperatively to 90 (IQR 20) postoperatively (p < 0.001). Similarly, KSS Function scores increased from 60 (IQR 26) to 93 (IQR 21) postoperatively (p < 0.001).
As expected with a restricted kinematic alignment technique, the HKA was corrected to 177 (IQR 5.8) postoperatively. without any statistically significant difference for mLDFA (89.0 ± 3.0 vs 89.9 ± 2.6; p = 0.57; Table 2). The mMPTA did differ between the pre- and postoperative situation (86.0 ± 3.6 vs 88.6 ± 2.2; p < 0.001). Blackburn Peel ratio increased slightly postoperatively from 0.65 ± 0.13 to 0.69 ± 0.16 (p = 0.023). On the axial radiographs, patellar position was central in 92%, although some tilt was observed in 5% and subluxation in 3% of cases.
Comparison between the preoperative and postoperative radiological parameters, range of motion and KSS scores.
In total there were 5 patients who suffered complications following their TKA (Table 3). PJI and arthrofibrosis were most common (1.6% for both groups separately), followed by aseptic loosening of a cementless femoral component (0.8%) and patellar dislocation (0.8%). The revision-free survival, which was 98% at 5 years, can be seen in Figure 1.
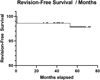 |
Figure 1 Kaplan Meier curve demonstrating revision-free survival rates over the follow-up period (Months). |
Overview of the complications observed during the 5 years of follow-up in this study.
Discussion
In current literature there is high focus on personalization in TKA, aiming to provide superior clinical outcomes and satisfaction. The findings of this study adds to that body of evidence demonstrating that deep-dish TKA yields excellent clinical outcomes and high patient satisfaction at a five-year follow-up, together with high implant survival. The insights gained from this study may guide future practices in TKA, particularly in the context of refining the combination between alignment strategies and implant design in an attempt to optimize patient satisfaction and clinical function.
Despite the strong clinical outcomes observed, our study has several limitations that must be acknowledged. First, its retrospective design introduces potential recall bias, as patient-reported satisfaction and function scores rely on subjective recollection rather than standardized prospective assessments. Second, while this study was conducted at a single center with high volume surgeons, the generalizability of our results to other institutions and patient populations might be limited. Multi-center trials with diverse cohorts would help confirm whether these outcomes are replicable across different surgical teams and healthcare settings. Third, no comparative analysis was performed analyzing differences between a different alignment philosophy or implant design. However, the discussion below aims to thoroughly assess the results of this study in light of current literature (Table 4).
Overview of the studies currently reporting clinical results or complications on deep-dish TKA.
The KSS Knee and KSS Function in this study were similar to scores reported in other studies assessing deep-dish TKA outcomes (Table 4). For example, several studies found that patients receiving deep-dish TKA demonstrated mean KSS Knee values between 85.5 and 94, depending on the specific implant system used [1, 2, 4, 19]. A retrospective study by Lefèvre et al. found that deep-dish designs showed median postoperative KSS scores of 91.5, which was not significantly different from a PS design [20]. Similarly, Shatrov et al. could not demonstrate any difference in clinical outcomes between their deep-dish cohort and matched CR cohort at 3-years postoperatively [2]. While deep-dish TKA theoretically could be associated with a risk of limited flexion due to its constraint, our findings suggest that functional outcomes remain excellent, further supporting its continued use in clinical practice [21]. Of course, these slight similarities and differences should be interpreted considering several factors, for example the study location, patient demographics, surgical protocol, postoperative pain management and rehabilitation.
A remarkable aspect of our findings is the 94% satisfaction rate, which is higher than that reported in many historical studies [22], as well as on deep-dish TKA (Table 4) [2, 3, 20]. One of the studies on deep-dish TKA by Lefèvre et al. was similar to our results with satisfaction rates around 94% at five years postoperatively, which is in contrast to the study of Shatrov et al. and Stirling et al., which has stated a dissatisfaction rate of 17% in their deep-dish TKA cohort at 3 and 1 years postoperatively, respectively [2, 3]. The study by Stirling et al. used a fixed bearing design, although there is no clear superiority of either fixed- or mobile bearing designs in current literature. However, an upward trend in satisfaction might be seen with more recently published studies, in particular when modern surgical, anesthesiology, and rehabilitation principles are applied.
One potential reason for the success of deep-dish TKA in our study is the use of restricted kinematic alignment, which appears to offer an optimal balance between mechanical and unrestricted kinematic alignment [11]. While traditional mechanical alignment ensures standardized component positioning, it does not always respect individual patient anatomy, which could lead to suboptimal kinematics and eventually, clinical outcomes [23, 24].
Recent studies have highlighted the benefits of restricted kinematic alignment. A study by Vendittoli et al. found that restricted kinematic alignment resulted in improved gait mechanics, quadriceps function, and patient-reported outcomes compared to strict mechanical alignment [11]. However, comparative trials evaluating alignment techniques with rotating-platform deep-dish TKA are currently lacking. Our study adds to the growing body of evidence by demonstrating that restricted kinematic alignment allows for excellent clinical outcomes and patient satisfaction in deep-dish TKA, further supporting its clinical relevance.
In general, the complication rate in this study was similar to other reported studies on rotating-platform TKA [25]. There was no tibial loosening seen, which theoretically might be a concern with the highly conforming insert. The rotating platform seems to protect the tibial component from early loosening, similar to the study by Stadler et al. [4]. While our study demonstrates excellent mid-term results, the long-term durability of deep-dish TKA remains an important question. Some prior reports have suggested that while deep-dish TKA provides good stability, the increased conformity may limit femoral rollback and reduce flexion capacity compared to more traditional designs [21]. Future research should focus on long-term survivorship, component wear, and revision rates beyond 10 years to determine whether these promising mid-term outcomes translate into durable, long-term success.
Conclusion
This study demonstrates that a rotating-platform deep-dish TKA with restricted kinematic alignment provides excellent mid-term outcomes, with high patient satisfaction, significant functional improvements, and a 98% revision-free survival at five years. Multicenter trials and extended follow-up beyond 10 years will help determine whether implant loosening might be an issue.
Funding
This research did not receive any specific funding.
Conflicts of interest
Author 1, Author 2 and Author 4 declare that they have no conflicts of interest. Author 3: Consultant for Corin. Author 5: Consultant for Stryker, Smith and Nephew, Heraeus. Institutional research support to Lepine and Amplitude. Editorial Board for Journal of Bone and Joint Surgery (Am).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author contribution statement
Author 1: Data analysis, Visualization, Writing original draft.
Author 2: Data collection, Data analysis, Reviewing and editing.
Author 3: Conceptualization, Data analysis, Reviewing and editing.
Author 4: Conceptualization, Data analysis, Reviewing and editing.
Author 5: Conceptualization, Data analysis, Reviewing and editing.
Ethics approval
This study received ethical approval from the Ethics committee of “anonymized” under the protocol number ICP-D106.02.
References
- Laskin RS, Maruyama Y, Villaneuva M, Bourne R (2000) Deep-dish congruent tibial component use in total knee arthroplasty: a randomized prospective study. Clin Orthop Relat Res 380, 36–44. https://doi.org/10.1097/00003086-200011000-00006. [CrossRef] [Google Scholar]
- Shatrov J, Sappey-Marinier E, Kafelov M, et al. (2022) Similar outcomes including maximum knee flexion between mobile bearing condylar-stabilised and fixed bearing posterior-stabilised prosthesis: a case control study. J Exp Orthop 9, 17. https://doi.org/10.1186/s40634-022-00456-0. [CrossRef] [PubMed] [Google Scholar]
- Stirling P, Clement ND, MacDonald D, et al. (2019) Early functional outcomes after condylar-stabilizing (deep-dish) versus standard bearing surface for cruciate-retaining total knee arthroplasty. Knee Surg Relat Res 31, 3. https://doi.org/10.1186/s43019-019-0001-7. [CrossRef] [PubMed] [Google Scholar]
- Stadler C, Hofstätter M, Luger M, et al. (2023) No component loosening of a cementless deep dish rotating platform knee at a 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 31, 969–978. https://doi.org/10.1007/s00167-022-07113-0. [CrossRef] [PubMed] [Google Scholar]
- MacDessi SJ, Oussedik S, Abdel MP, et al. (2023) The language of knee alignment: updated definitions and considerations for reporting outcomes in total knee arthroplasty. Bone Joint J 105-B, 101. https://doi.org/10.1302/0301-620X.105B2.BJJ-2023-00028. [CrossRef] [PubMed] [Google Scholar]
- Howell SM, Shelton TJ, Hull ML (2018) Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty 33, 3678–3684. https://doi.org/10.1016/j.arth.2018.07.020. [CrossRef] [PubMed] [Google Scholar]
- Sterneder CM, Faschingbauer M, Haralambiev L, et al. (2024) Why kinematic alignment makes little sense in valgus osteoarthritis of the knee: a narrative review. J Clin Med 13, 1302. https://doi.org/10.3390/jcm13051302. [CrossRef] [PubMed] [Google Scholar]
- Brown NM, Lingampalli N, Hellman MD (2024) Intraoperative challenges of the kinematic knee. Orthop Clin North Am 55, 27–32. https://doi.org/10.1016/j.ocl.2023.07.001. [CrossRef] [PubMed] [Google Scholar]
- Courtney PM, Lee G-C (2017) Early outcomes of kinematic alignment in primary total knee arthroplasty: a meta-analysis of the literature. J Arthroplasty 32, 2028–2032. https://doi.org/10.1016/j.arth.2017.02.041. [CrossRef] [PubMed] [Google Scholar]
- Blakeney WG, Vendittoli P-A (2020) Restricted kinematic alignment: the ideal compromise? In: Personalized hip and knee joint replacement. Rivière C, Vendittoli P-A, EditorsCham (CH), Springer. [Google Scholar]
- Vendittoli P-A, Martinov S, Blakeney WG (2021) Restricted kinematic alignment, the fundamentals, and clinical applications. Front Surg 8, 697020. https://doi.org/10.3389/fsurg.2021.697020. [CrossRef] [PubMed] [Google Scholar]
- Devane PA, Horne JG (1999) Assessment of polyethylene wear in total hip replacement. Clin Orthop Relat Res 369, 59–72. [CrossRef] [Google Scholar]
- Charnley J (1972) The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br 54, 61–76. [CrossRef] [Google Scholar]
- Debette C, Parratte S, Maucort-Boulch D, et al. (2014) French adaptation of the new Knee Society Scoring System for total knee arthroplasty. Orthop Traumatol Surg Res 100, 531–534. https://doi.org/10.1016/j.otsr.2014.03.025. [CrossRef] [PubMed] [Google Scholar]
- Parvizi J, Tan TL, Goswami K, et al. (2018) The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty 33, 1309–1314. https://doi.org/10.1016/j.arth.2018.02.078. [CrossRef] [PubMed] [Google Scholar]
- Healy WL, Della Valle CJ, Iorio R, et al. (2013) Complications of total knee arthroplasty: standardized list and definitions of the Knee Society. Clin Orthop Relat Res 471, 215–220. https://doi.org/10.1007/s11999-012-2489-y. [PubMed] [Google Scholar]
- Putman S, Boureau F, Girard J, et al. (2019) Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res 105, S43–S51. https://doi.org/10.1016/j.otsr.2018.04.028. [CrossRef] [PubMed] [Google Scholar]
- Khow YZ, Liow MHL, Goh GS, et al. (2022) Defining the minimal clinically important difference for the knee society score following revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30, 2744–2752. https://doi.org/10.1007/s00167-021-06628-2. [CrossRef] [PubMed] [Google Scholar]
- Czekaj J, Fary C, Gaillard T, Lustig S (2017) Does low-constraint mobile bearing knee prosthesis give satisfactory results for severe coronal deformities? A five to twelve year follow up study. Int Orthop 41, 1369–1377. https://doi.org/10.1007/s00264-017-3452-z. [CrossRef] [PubMed] [Google Scholar]
- Lefèvre M, Cavailhès J, Ferri C, et al. (2022) CORIN KneeTec DeepDishTM: functional outcomes after a follow-up of 12 months and comparison with the STRYKER Triathlon PS. Acta Orthop Belg 88, 61–71. https://doi.org/10.52628/88.1.09. [CrossRef] [PubMed] [Google Scholar]
- Machhindra MV, Kang JY, Kang YG, et al. (2015) Functional outcomes of a new mobile-bearing ultra-congruent TKA system: comparison with the posterior stabilized system. J Arthroplasty 30, 2137–2142. https://doi.org/10.1016/j.arth.2015.06.011. [CrossRef] [PubMed] [Google Scholar]
- Singh M, Harary J, Schilling PL, Moschetti WE (2024) Patient satisfaction is nearly 90% after total knee arthroplasty; we are better than we were. J Arthroplasty 40, P1521–1525. https://doi.org/10.1016/j.arth.2024.11.038. [Google Scholar]
- Hirschmann MT, Moser LB, Amsler F, et al. (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27, 1394–1402. https://doi.org/10.1007/s00167-019-05509-z. [CrossRef] [PubMed] [Google Scholar]
- Pangaud C, Siboni R, Gonzalez J-F, et al. (2024) Restoring the preoperative phenotype according to the coronal plane alignment of the knee classification after total knee arthroplasty leads to better functional results. J Arthroplasty 39, 2970–2976. https://doi.org/10.1016/j.arth.2024.06.012. [CrossRef] [PubMed] [Google Scholar]
- Hao D, Wang J (2021) Fixed-bearing vs mobile-bearing prostheses for total knee arthroplasty after approximately 10 years of follow-up: a meta-analysis. J Orthop Surg Res 16, 437. https://doi.org/10.1186/s13018-021-02560-w. [CrossRef] [PubMed] [Google Scholar]
Cite this article as: Vermue H, Mesnard G, Servien E, Batailler C & Lustig S (2025) Rotating-platform deep-dish total knee arthroplasty with restricted kinematic alignment: Five-year clinical and functional outcomes. SICOT-J 11, 33. https://doi.org/10.1051/sicotj/2025018.
All Tables
Comparison between the preoperative and postoperative radiological parameters, range of motion and KSS scores.
Overview of the complications observed during the 5 years of follow-up in this study.
Overview of the studies currently reporting clinical results or complications on deep-dish TKA.
All Figures
 |
Figure 1 Kaplan Meier curve demonstrating revision-free survival rates over the follow-up period (Months). |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


